Progesterone often drops first in perimenopause - not estrogen. Learn why hormone tracking, and individualized HRT, may be the smarter choice.

Editor’s Note:
Perimenopause can feel like a puzzle no one gave you the picture for: mood swings, weight gain, restless nights - all while ads promise quick fixes and “perfect balance.” This is your compass to cut through the noise, understand what’s really happening in your body, and find practical, science-backed ways to restore balance on your own terms.
Why Standard Hormone Therapy Can Miss the Mark in Perimenopause
It’s happening more often: women in perimenopause are offered full hormone replacement therapy (HRT) as if it were a standard prescription - no precise testing, no real conversation about which hormone is changing first, or which stage they’re actually in - or where those high estrogen levels might actually be coming from, whether from natural ovarian surges or from slower clearance and recirculation through the liver and gut.
Lately, I’ve been seeing more and more glossy ads targeting women in their 40s, promoting “perfectly balanced” hormone blends - usually a fixed combination of estradiol and progesterone — as if one ratio could work for every woman, at every stage. It’s an appealing promise, but also a risky oversimplification.
But here's the issue:
Perimenopause isn't menopause.
And menopause isn't postmenopause.
These are three distinct stages of a woman's life*, each with unique different hormonal dynamics, symptoms, and risks. Treating them all the same not only ignores the nuanced early signs of hormone imbalance that can alter the course of your well-being, but also contradicts the very principles of personalized, responsible medicine.
Progesterone Is Often the First Messenger - Not Estrogen
In early perimenopause, progesterone decline is typically the first hormonal shift to occur—long before estrogen significantly dips. Why? Because progesterone depends on ovulation, and as cycles become more erratic, ovulation becomes inconsistent or stops entirely.
Without ovulation, your body loses its main source of progesterone in the luteal phase, leaving only trace amounts from the adrenal glands.
No ovulation = no progesterone
This silent hormonal shift can cause:
- Sleep disturbances
- Irritability and anxiety
- Mood swings
- New belly weight gain
- Reduced stress resilience
These symptoms are often partly or fully misattributed to estrogen deficiency, leading to premature or unbalanced estrogen therapy.
But this phase is not about estrogen dominance either—it’s about losing the calming, anchoring effect of progesterone.
Progesterone is the hormone of calm. Its decline is often associated with the emotional tipping point of perimenopause - well before periods become irregular or stop altogether.
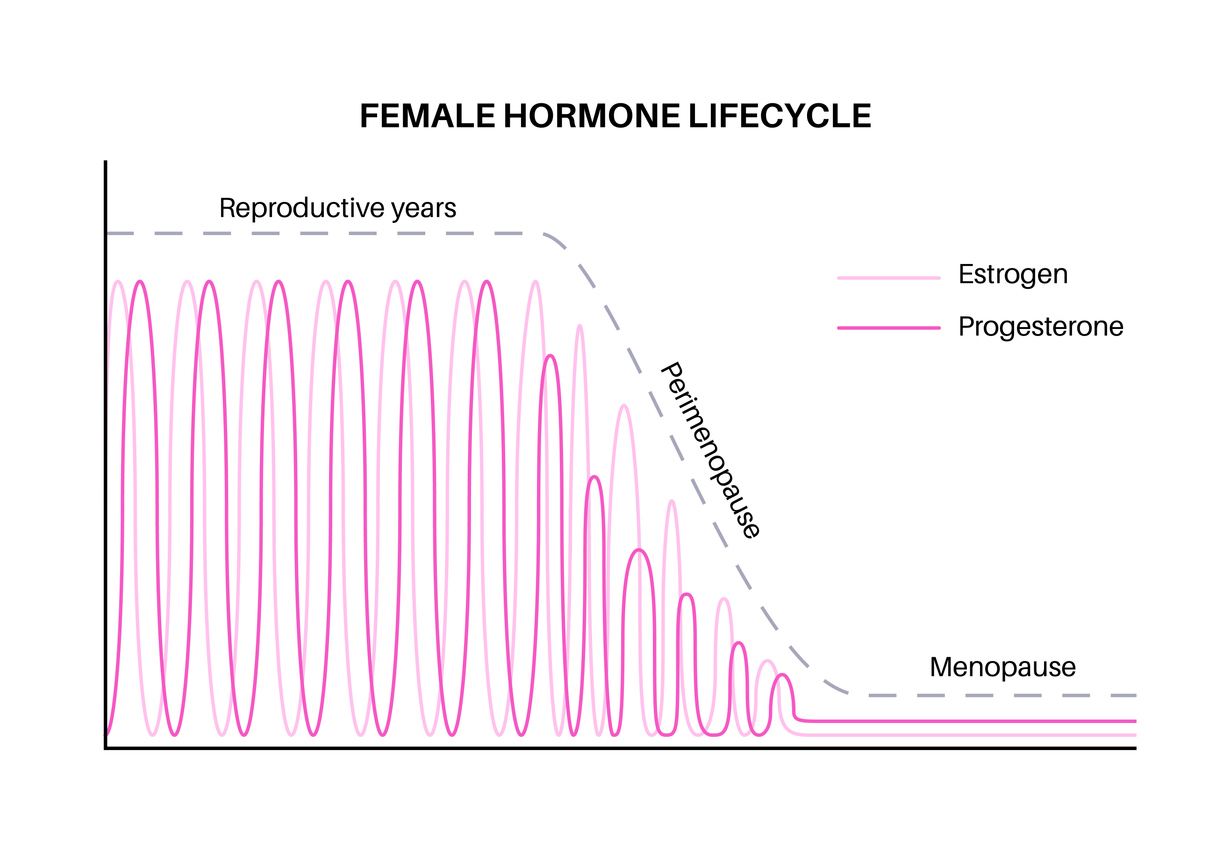
Disclaimer: This chart illustrates typical hormone patterns and is for educational purposes only. Individual hormone levels and changes may vary. It is not a substitute for professional medical advice, diagnosis, ort reatment.
Tracking Progesterone and Estrogen Is Not Optional—It’s Essential
A responsible approach to HRT begins not with a pill, patch or cream but with a journal — and regular hormone tests. Especially in perimenopause, women should:
- Track mood and cycle-related symptoms — for example, journaling changes in energy, sleep quality, mood stability, PMS symptoms, and menstrual flow patterns (see our,guide: “Mood & Symptom Tracking for Hormone Health” (coming soon) for practical templates and what patterns to look for).
- Measure progesterone and estrogen levels regularly (see our guide: “How to Test Progesterone?” (coming soon) for timing, test options, and interpretation tips). In women with irregular cycles, the optimal testing day can be harder to pinpoint, so results should always be interpreted in context.
- Address liver metabolism and detox pathways — in other words, support the liver’s metabolic processes that are responsible for breaking down and eliminating hormones (see our article: “The Liver-Hormone Connection: A Natural Way to Reduce Perimenopause Symptoms (Part I)” and "The Liver-Hormone Connection: A Natural Way to Reduce Perimenopause Symptoms (Part 2)" for how the liver processes estrogen and progesterone, and practical ways to support it) - especially if PMS, mood swings, or histamine intolerance are present.
Why Tracking Progesterone and Estrogen Is Essential?
Because without this knowledge, you’re guessing. You may have symptoms from low progesterone while your estrogen is still high - and adding more estrogen could make things worse.
Regular testing may help you understand where your symptoms come from, whether bioidentical progesterone timed to your cycle could help, or whether the “miracle cream” you saw advertised might actually be the wrong choice for you.
And remember - progesterone is not just a “pregnancy hormone.” It’s also a neuroactive steroid that:
- Calms the nervous system by acting on GABA receptors (= gamma-aminobutyric acid receptors — the brain’s main “calm-down” switches that help reduce overactivity and promote relaxation)
- Supports deeper, more restorative sleep (by lowering nighttime cortisol and helping your brain shift into slower, more restful brainwave patterns)
- Helps stabilize mood and emotional resilience (reducing sensitivity to stress signals and supporting balanced neurotransmitter activity)
- Plays a role in blood sugar regulation (by improving insulin sensitivity and helping to prevent large spikes and crashes in glucose levels)
When you track your hormones, you’re not simply gathering numbers. You’re learning the language of your body. You begin to see the patterns behind your symptoms, understand whether they point to progesterone decline, estrogen dominance, or another imbalance - and recognize early warning signs before they become bigger issues.
That knowledge gives you the power to respond: to support your hormones with the right nutrients, adjust your lifestyle, address liver metabolism, or, when needed, work with a clinician to target treatment precisely - rather than relying on a “miracle cream” that may not match your actual needs.
Estradiol in Perimenopause: A Nuanced Approach
Perimenopause isn’t a steady drop in estrogen - it’s a hormonal rollercoaster. Estradiol can fluctuate significantly from one week to the next, and at times may even be higher than in earlier reproductive years before dropping again (fluctuations may also be influenced by how efficiently your liver and gut clear and recycle estrogen - see our article: “The Liver-Hormone Connection: A Natural Way to Reduce Perimenopause Symptoms (Part I)” and "The Liver-Hormone Connection: A Natural Way to Reduce Perimenopause Symptoms (Part 2)".
That’s why you can have estrogen dominance symptoms like breast tenderness, bloating, heavy periods right alongside low-estrogen symptoms (night sweats, dryness).
Why starting estradiol supplementation during perimenopause is so tricky:
- Fluctuations mean supplementation could cause excess during natural highs
- Unopposed estrogen (= estrogen without the balancing effect of progesterone) can lead to a thicker-than-normal uterine lining, a condition called endometrial hyperplasia, which may raise health risks over time in women who still have their uterus (have not had a hysterectomy) .
- Many symptoms commonly attributed to perimenopause may not stem from estrogen loss alone. Progesterone decline often plays a key role — but so can imbalances in the thyroid, adrenal glands, or pancreas, and even hypothalamic amenorrhea. To understand how the brain and these glands work together — and why many “hormonal” symptoms actually begin in the hypothalamus — explore our article Why So Many ‘Hormonal’ Symptoms Begin in the Brain
When estradiol supplementation may be considered:
- Consistently low estradiol on repeat tests plus matching symptoms
- Significant quality-of-life disruption despite balanced progesterone levels and lifestyle support
- Always with progesterone protection and medical supervision (unless the uterus has been removed, in which case endometrial protection is not required, though some clinicians may still prescribe progesterone for non-endometrial benefits)
Remember, in perimenopause, estradiol use is not a universal solution. Estradiol supplementation should be targeted and personalized, tailored to your specific needs and symptoms. Never assume that estradiol use is automatic or standard for everyone.
Estrogen Without Progesterone? That’s a Risky Equation.
Later in life - especially in menopause or postmenopause - supporting declining estrogen levels can feel like a gift: more energy, improved skin elasticity, fewer hot flashes. But there's a crucial detail often overlooked:
For women with an intact uterus, estrogen therapy should always be balanced with progesterone to protect the uterine lining.
Estrogen's role is to build. It thickens the uterine lining, influences breast tissue, and stimulates cellular activity. That in itself isn't a problem—unless that growth remains unopposed (so called unopposed estrogen therapy).
Progesterone brings balance to the picture.
It moderates estrogen's effects on tissue, keeping cell proliferation in line with estrogen's support of a safe hormonal rhythm. When progesterone is missing, the balance is disrupted.
Missing Progesterone - What does that mean in real life?
The endometrium may continue to build without shedding, increasing the risk for hyperplasia or, over time, cancer. Breast tissue may become more sensitive to proliferative signals. Even insulin sensitivity and fat metabolism can be affected when estrogen dominates without its natural counterpart.
The Female Endocrine System Is Complex & Requires Thoughtful Navigation
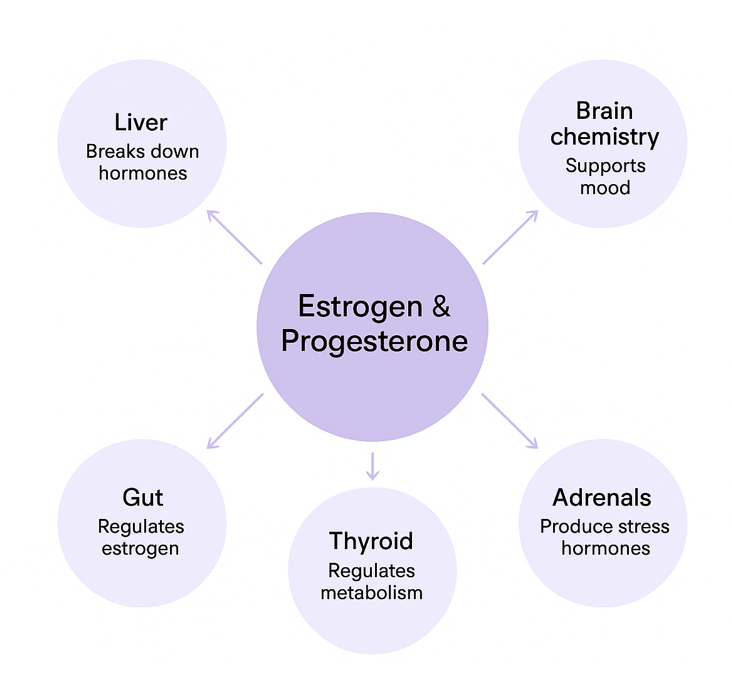
Hormones don’t work in isolation. Your hormones aren’t lone operators — they’re part of a complex network that includes your liver, gut, thyroid, adrenals, and brain chemistry.
- Liver: Acts like your body’s hormonal filter. It breaksdown excess estrogen and metabolizes progesterone. If liver estrogen metabolism pathways are sluggish — from poor diet, alcohol, certain medications, or inflammation — hormones can recirculate in active form, leading to symptoms like bloating, breast tenderness, and mood swings.
- Gut: Houses the estrobolome — a collection of gut bacteria that help regulate estrogen levels. Emerging research suggests that dysbiosis or chronic constipation can cause estrogen buildup, tipping the balance against progesterone.
*Hormonal balance is a whole-body affair. Your liver,gut, thyroid, adrenals, and brain chemistry are all part of the sameconversation — and ignoring one can disrupt them all.
- Thyroid: Works hand in hand with sex hormones to regulate metabolism and energy. Low thyroid function can worsen progesterone deficiency symptoms like fatigue, brain fog, and weight gain.
- Adrenals: Your stress-response glands also produce small amounts of progesterone and estrogen precursors. Chronic stress can divert resources away from sex hormone production, accelerating imbalance.
- Brain Chemistry: Progesterone acts as a neuroactive steroid, calming overactive neurons via GABA receptors. Low levels can mean more anxiety, poor sleep, and difficulty handling stress.
Why Holistic HRT Approach Matters for You?
If HRT strategy focuses only on replacing hormones without supporting these systems - especially liver detox and inflammation control — it’s like filling a bathtub with the drain open. You won’t get sustainable results, and in some cases, you may worsen the imbalance. Addressing these connections first can make HRT more effective, safer, and tailored to what your body actually needs.
Conclusion: Thriving Through Perimenopause Starts With the Right Balance
Perimenopause isn’t a cliff you suddenly fall off - it’s a winding road with curves you don’t see until you’re in them. Along the way, your hormones won’t all shift in the same direction at the same pace. Progesterone decline is often the first to quietly step back, and when it does, the changes you feel can be just as real - and just as disruptive - as those in menopause.
That’s why personalized HRT is crucial. Your body doesn’t need more of everything - it requires the proper support at the right time. Be cautious with treatments that bundle multiple hormones together without targeted testing, especially when estrogen vs progesterone balance isn’t checked.
With personalized HRT, you can be reassured that your treatment plan is tailored to your specific needs, giving you the confidence to navigate perimenopause with ease.
Equally important is actively supporting the two systems that clear estrogen from your body: the liver, which metabolizes it, and the gut, which helps decide whether it’s reabsorbed or eliminated. (see our guide “The Liver–Gut Connection: A Natural Way to Reduce Perimenopause Symptoms” for strategies that may help delay or reduce perimenopausal symptoms). In perimenopause, both systems can become less efficient, potentially intensifying estrogen-related symptoms. Supporting healthy estrogen metabolism and a balanced gut microbiome can make HRT more effective and reduce unwanted side effects. In some women, improving liver metabolism and gut health may even help smooth out estrogen spikes enough to delay or reduce the need for HRT - especially in the earlier stages of perimenopause.
Empower yourself by tracking your cycle and knowing your hormone levels. Support your liver, gut, thyroid, adrenals, and brain chemistry - because all of them work together.
The goal isn’t just to get through perimenopause. It’s to feel well, think clearly, and keep thriving in the years ahead.
Key Takeaways: Why HRT Isn’t a Universal Solution — and Why Progesterone and Liver Health Deserve More Attention
- Perimenopause ≠ Menopause ≠ Postmenopause –these life stages are hormonally and symptomatically distinct, and require different approaches.
- Progesterone often declines first –this drop frequently happens before estrogen decreases, as irregular cycles lead to fewer ovulations.
- Symptoms can be misleading –sleep issues, mood swings, or weight gain in perimenopause are often linked to low progesterone, not necessarily to low estrogen.
- Estrogen without progesterone is risky –in women with a uterus, unopposed estrogen increases the risk of endometrial hyperplasia.
- Hormonelevels fluctuate widely –estradiol can sometimes be higher than in earlier reproductive years before it drops permanently.
- Liver and gut health matter –both play a key role in breaking down and clearing estrogen, influencing symptoms and HRT safety.
- Targeted hormone testing is essential –regularly measuring progesterone and estradiol (ideally ~7 days afterovulation) helps personalize therapy.
- Lifestyle counts – nutrition, stress management, liver support, gut health, and cycle tracking can ease symptoms and sometimes delay the need for HRT.
*Note: While awoman’s hormonal journey typically includes five main phases (puberty,reproductive years, perimenopause, menopause, and postmenopause), this articlefocuses on the final three—where hormone therapy is most frequently consideredand most often misapplied.
Disclaimer: This article is intended for educational purposes only and does not constitute medical advice. Please consult your healthcare provider before initiating or modifying any form of hormone therapy.

Written by Elena Brull, FNR, Functional Nutrition Researcher & Women’s Health Journalist
About the Author
Elena Brull, FNR, is a Functional Nutrition Researcher and Women’s Health Journalist specializing in integrative approaches to hormonal balance, nutrition, and longevity. Her work combines evidence-based insights with holistic health principles to help women understand their biology and live in rhythm with it. She writes from a non-clinical, educational perspective — with the intention to inform and empower, not to diagnose or prescribe.
References:
Burger, H. G., Hale, G. E., Robertson, D. M., & Dennerstein, L. (2007). A review of hormonal changes during the menopausal transition: Focus on findings from the Melbourne Women’s Midlife Health Project. Human Reproduction Update,13(6), 559–565. https://academic.oup.com/humupd/article-abstract/13/6/559/682984
Hale, G. E.,Robertson, D. M., & Burger, H. G. (2009). The perimenopausal woman: Endocrinology and management. Journal of Steroid Biochemistry and Molecular Biology, 114(1–2), 118–126. https://www.sciencedirect.com/science/article/abs/pii/S0960076009000065
Pluchino N, Luisi M, Lenzi E, et al. Progesterone and progestins: effects on brain, allopregnanolone and beta-endorphin 2006 Dec;102(1–5):205–213. PubMedPMID: 17052903 https://pubmed.ncbi.nlm.nih.gov/17052903
Freeman, E. W., etal. (2007). Associations of hormones and menopausal status with depressed mood in women with no history of depression. Archives of General Psychiatry,63(4), 375–382. https://jamanetwork.com/journals/jamapsychiatry/fullarticle/209523
Henderson BE, RossRK, Judd HL, et al. (1982). Estrogenic hormones in the pathogenesis ofendometrial cancer. Journal of the National Cancer Institute, 68(1),127–134. https://pubmed.ncbi.nlm.nih.gov/3358913
National CancerInstitute. (2024). Endometrial Cancer Prevention (PDQ®)–Health ProfessionalVersion. National Cancer Institute.
https://www.cancer.gov/types/uterine/hp/endometrial-prevention-pdq
American CancerSociety. (2023). Endometrial Cancer Risk Factors. American CancerSociety.
https://www.cancer.org/cancer/types/endometrial-cancer/causes-risks-prevention/risk-factors.html
Wikipedia contributors. (2024). Hormone replacement therapy. In Wikipedia.
https://en.wikipedia.org/wiki/Hormone_replacement_therapy
Wikipedia contributors. (2024). Estrogen (medication). In Wikipedia. https://en.wikipedia.org/wiki/Estrogen_(medication)
Santoro, N., et al.(2013). Menopausal transition: Linking endocrine changes to symptoms in the Study of Women’s Health Across the Nation. Menopause,20(11), 1131–1139. https://doi.org/10.1097/GME.0b013e318287342d
Writing Group for theWomen’s Health Initiative Investigators. (2002). Risks and benefits of estrogenplus progestin in healthy postmenopausal women: Principal results from the Women’s Health Initiative randomized controlled trial. JAMA, 288(3),321–333. https://jamanetwork.com/journals/jama/fullarticle/195120
Manson, J. E., et al. (2013). Menopausal hormone therapy and health outcomes during the intervention and extended post stopping phases of the Women’s HealthInitiative randomized trials. JAMA,310(13), 1353–1368.
https://jamanetwork.com/journals/jama/fullarticle/1745676
Clarke, C. L., & Sutherland, R. L. (1990). Progestin regulation of cellular proliferation. Endocrine Reviews, 11(2), 266–301. https://academic.oup.com/edrv/article-abstract/11/2/266/2548574
Key, T. J., &Pike, M. C. (1988). The role of oestrogens and progestagens in the epidemiology and prevention of endometrial cancer. European Journal of Cancer &Clinical Oncology, 24(1), 29–43.
https://www.sciencedirect.com/science/article/abs/pii/0277537988901733
Della Torre, S.,Mitro, N., & Maggi, A. (2016). The liver in the regulation of energy metabolism: A perspective on the interplay between estrogen and the liver. Endocrine Reviews, 37(4), 303–321. PMCID:PMC4600502
Coombes, Z., Plant,K., Freire, C., Basit, A. W., Butler, P., Conlan, R. S., & Gonzalez, D.(2021). Progesterone metabolism by human and rat hepatic and intestinal tissue. Pharmaceutics, 13(10), 1707. https://pmc.ncbi.nlm.nih.gov/articles/PMC8537901
Discover Products to Support Your Health & Well-Being
Science Spotlight
Curious About the Science behind this Article?
The Liver in Regulation of Energy Metabolism: A Perspective on the Interplay Between Estrogen and the Liver (PMID: 26454069, PMC4600502)
The liver is not only a nutrient-processing organ - it is also a central target and regulator for sex hormones such as estrogens. Estradiol directly influences the liver’s glucose and lipid metabolism, while the liver, in turn, is essential for metabolizing and clearing sex hormones. This two-way interaction impacts weight, insulin sensitivity, fat distribution, and the risk of metabolic disease.
Takeaway
"Your liver isn’t just your body’s detox organ - it’s an active player in your hormonal balance. In peri- and postmenopause, its interaction with estradiol can determine whether you store or burn energy, and whether fat is deposited or mobilized."