Why the Liver-Homone Axis Matters More After 40

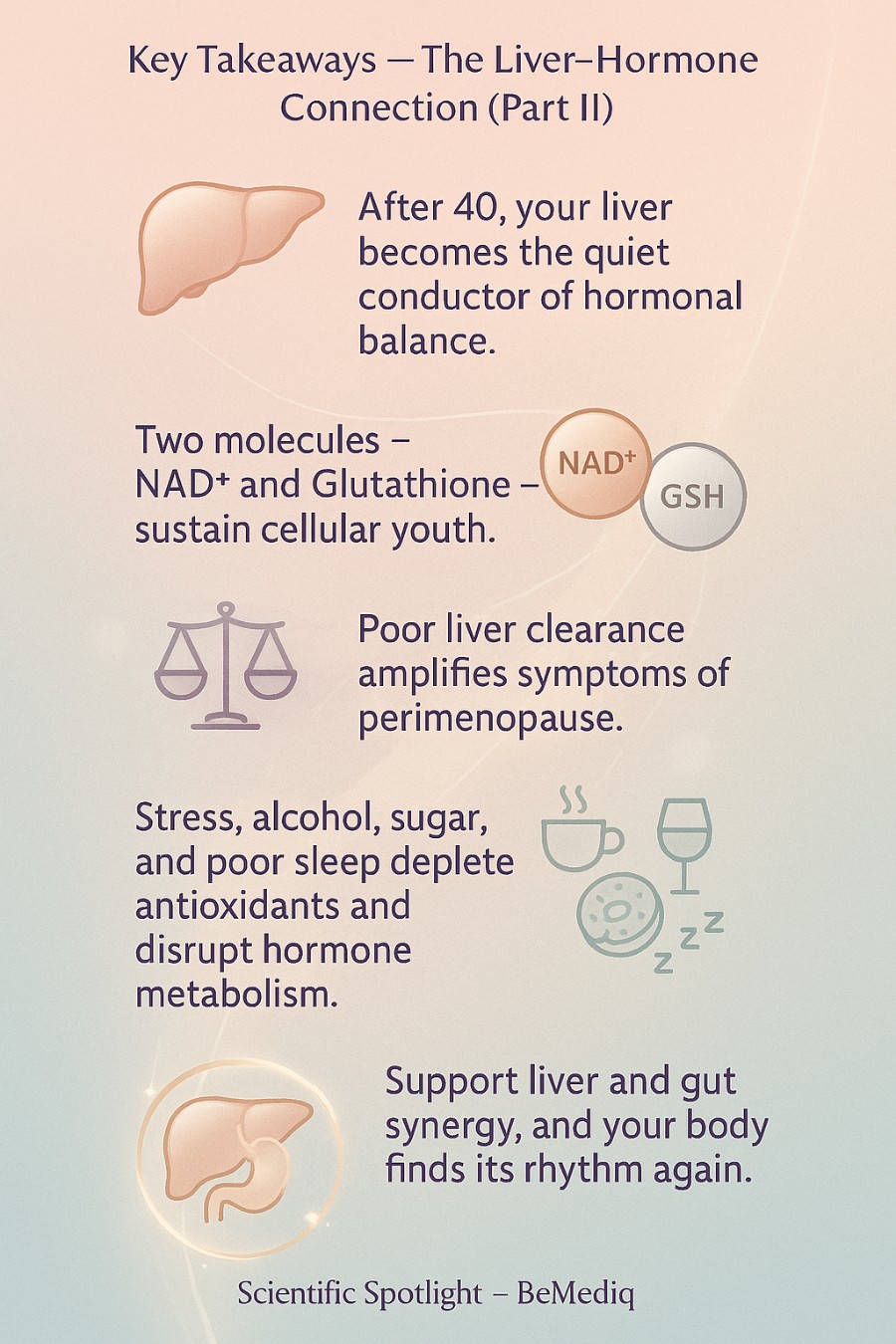
Key Takeaways — The Liver–Hormone Connection (Part II)
- After 40, your liver becomes the quiet conductor of hormonal balance.
How well it clears hormones matters more than how much you produce. - Two molecules — NAD⁺ and Glutathione — sustain cellular youth.
Both decline with age, affecting energy, skin, and mood regulation. - Poor liver clearance amplifies symptoms of perimenopause.
Estrogen dominance, bloating, and fatigue often stem from hormonal buildup, not deficiency. - Modern life adds to the load.
Stress, alcohol, sugar, and poor sleep deplete antioxidants and disrupt hormone metabolism. - Support liver and gut synergy.
Nutrients, antioxidants, and medical-grade NAD⁺ or Glutathione help restore the body’s natural rhythm. - Graceful aging begins where true detoxification takes place — within your cells.
When the liver regains its rhythm, your hormones — and your vitality — follow.
After 40 — Where Hormonal Change Meets Renewal
The years after 40 can be extraordinary — a time of depth, renewal, and rediscovery.
Yet, it’s also a time when your body begins to whisper for more attention.
Not just the physical body — but how you feel inside it.
At this stage, subtle biological transitions begin to unfold: changes in energy, skin tone, metabolism, and emotional rhythm.
Being prepared for them — and knowing how to work with your biology, not against it — can turn this chapter into one of vitality and power rather than decline.
In many cultures, turning forty marks the beginning of real life — a time of wisdom and confidence.
And yet, biology follows its own rhythm.
Understanding those rhythms, and learning to collaborate with them, becomes the key to preserving youthfulness — not as an illusion, but as a living expression of balance.
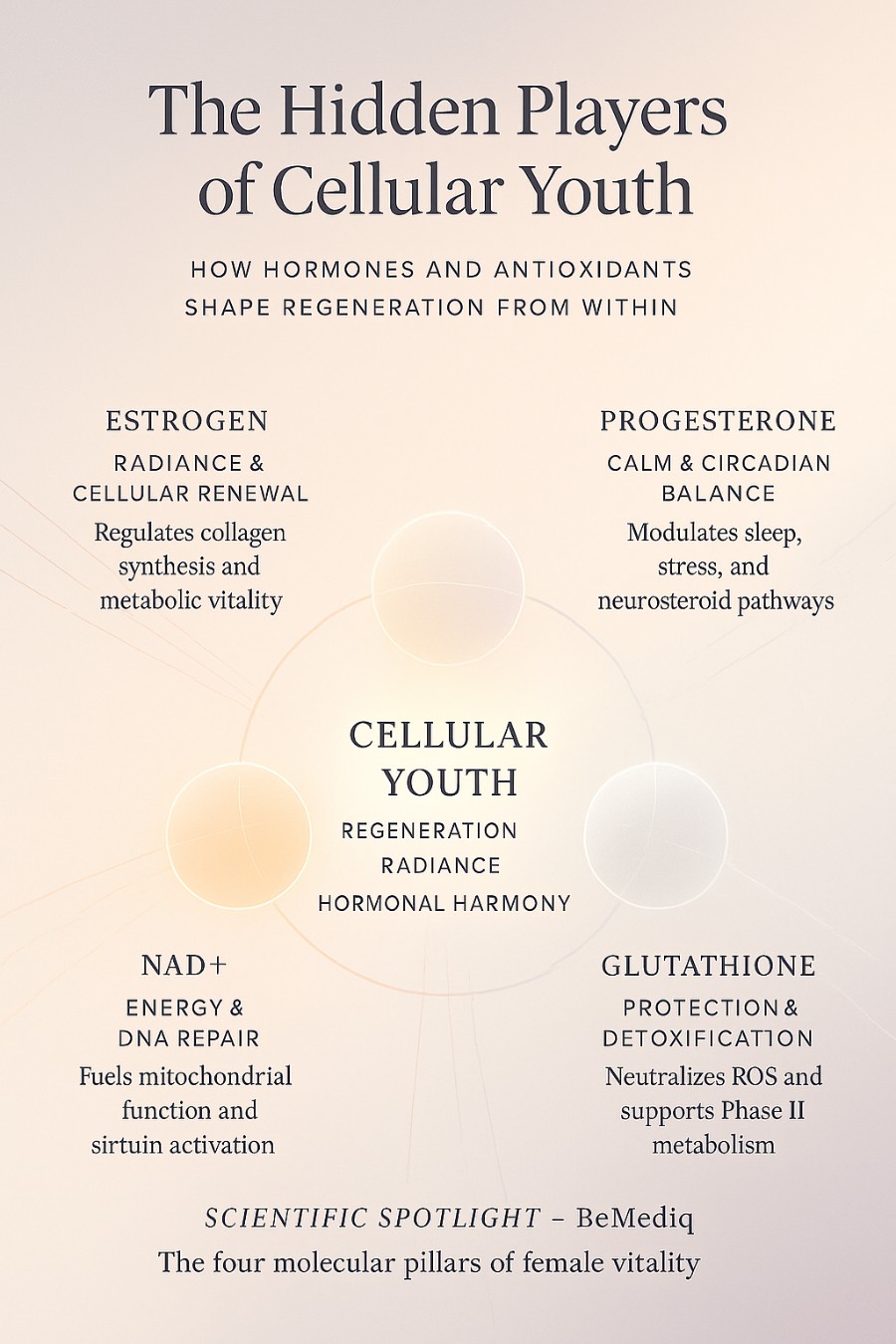
The Hidden Players of Cellular Youth
For educational purposes only. This visual does not provide medical advice and is not intended to diagnose, treat, cure, or prevent any disease. Always consult a qualified healthcare provider before making health-related decisions.
Two biological forces silently guard our vitality:
• The antioxidants your body produces on its own — NAD⁺ and Glutathione.
• The hormones that define your feminine rhythm — estrogen and progesterone.
These four act like the pillars of regeneration and radiance — supporting skin elasticity, cellular repair, emotional equilibrium, and metabolic energy.
But after 40,something begins to change.
Your body’s ability to produce these powerful molecules naturally starts to decline — NAD⁺ and glutathione levels can drop by up to 50–60% compared with your twenties [1][2].
You might notice it first in subtle ways: skin that loses some of its glow,energy that fades faster, slower recovery after stress, or a hint of brain fog where once there was clarity.
The Liver: The Core Generator
Here’s where the connection becomes essential.
Both NAD⁺ and Glutathione are primarily produced and recycled in the liver [3][4]— the organ that not only detoxifies external toxins but also manages the internal chemistry of renewal.
When liver functionis optimal, these antioxidants protect your cells from oxidative stress, support detoxification enzymes, and sustain the regeneration of tissues — including your skin, brain, and hormonal system [5] [6].
But when the liver becomes burdened by stress, alcohol, poor diet, or chronic inflammation, its ability to maintain these molecules weakens [7].
And with it, so does the body’s resilience — aging begins to accelerate, long before it’s biologically necessary [8].
Hormones and the Liver: A Two-Way Dialogue
The liver doesn’t just process nutrients — it’s also where estrogen, progesterone, testosterone, and cortisol are metabolized and cleared [9] [10].
Glutathione, often called the body’s master antioxidant, is also one of the main catalysts in the liver’s detoxification process [11].
When its levels drop, hormonal balance becomes harder to maintain — not because the body can’t produce hormones, but because it struggles to let go of what’s no longer needed.
When glutathione levels are low, this clearance slows [12].
Hormones that should have faded linger longer, creating what’s often described as estrogen dominance or androgen excess — the imbalance behind many familiar midlife symptoms:
bloating, tender breasts, mood swings, stubborn belly fat, hormonal acne, and hair thinning.
As discussed in PartI of this series, uncleared hormones distort the body’s rhythm, leading to emotional turbulence, metabolic sluggishness, and that wired-but-tired feeling so many women recognize.
A New Chapter in Collaboration
After 40, the goal isn’t to fight biology — it’s to collaborate with it.
By supporting your liver’s natural detox and regeneration pathways, you also support hormonal clarity, cellular energy, and emotional steadiness.
This is the quiet science of graceful longevity — where NAD⁺, glutathione, and hormone metabolism form a living triad that sustains vitality.
Your body isn’t “over the hill.”
It’s simply inviting you to evolve — to align with the deeper rhythm that’s been guiding you all along.
BeMediq Preventive Insight
The decline of liver-generated antioxidants like NAD⁺ and Glutathione after 40 may influence how efficiently your body clears hormones. Supporting liver health through nutrition, sleep, and stress balance helps maintain both cellular renewal and hormonal harmony.
Perimenopause: A Whole-Body Recalibration
Let’s take a closerlook at perimenopause — what truly happens beneath the surface, how yourhormones evolve in each stage, and why your liver and gut suddenly carry a heavier biological workload than ever before.
The Three Phases of Transition — What Really Happens in Perimenopause
Perimenopause isn’t a single moment; it’s a gradual hormonal symphony that unfolds in three overlapping stages — each one subtly reshaping how your body produces, circulates, and clears hormones.
And behind every hormonal note stands your liver, quietly working to keep the rhythm steady.
1. Early Perimenopause — The Subtle Shift
In the early stage, menstrual cycles may still appear regular, but ovulation becomes less predictable.
Estrogen remains relatively stable — even elevated at times — while progesterone begins to waver or drop because it’s only produced after ovulation.
This creates what endocrinologists call relative estrogen dominance [13] [14]: not necessarily because there’s too much estrogen, but because there’s not enough progesterone to balance it.
The result: more intense PMS, restless sleep, breast tenderness, water retention, and emotional sensitivity.
Since estrogen levels can stay higher for longer, your liver’s detox pathways already start to work overtime, processing repetitive peaks of unopposed estrogen.
2. Late Perimenopause — The Rollercoaster Phase
As ovarian follicle reserves decline, estrogen output becomes erratic and unpredictable — soaring one month, plunging the next [15] [16].
This stage brings hot flashes, night sweats, irregular or heavier cycles, and sudden mood swings.
Progesterone, the hormone that once brought calm and stability, is often too low to counter balance these spikes.
Your liver now faces surges of estrogen and cortisol to detoxify — while also managing increased oxidative stress.
When its detox capacity is strained by poor nutrition, alcohol, stress, or nutrient depletion, these hormonal waves start colliding.
That’s when symptoms like bloating, irritability, and fatigue become more pronounced, even in women who’ve always felt resilient.
3. Postmenopause — The New Baseline
Once 12 consecutive months have passed without a menstrual period, ovarian estrogen and progesterone levels remain chronically low [17] [18].
The body must now rely on peripheral hormone conversion — in fat tissue, adrenals, and the liver itself — to maintain essential estrogen activity for bone, brain, and cardiovascular function.
If the liver’s metabolic function is sluggish, these conversions become inefficient.
That’s when many women notice metabolic slowdown, changes in fat distribution (especially around the waist), elevated LDL cholesterol, or higher blood sugar [19].
This is not just about aging — it’s about how effectively your body’s biochemical systems adapt to a new equilibrium.
Why the Liver Carries the Weight of the Perimenopause?
The liver isn’t just a detox organ — it’s a metabolic regulator that helps determine how long hormones stay active in your system and how efficiently they’re cleared once their job is done.
Every molecule of estrogen, progesterone, cortisol, and thyroid hormone must pass through the liver’s enzymatic pathways for activation or clearance.
During perimenopause,when hormone levels oscillate wildly, the liver’s workload spikes: it must clear hormonal surges one week, and compensate for deficiencies the next.
This back-and-forth rhythm uses up vital cofactors like glutathione, B vitamins, magnesium, and NAD⁺ [20] [21].
At the same time, natural declines in NAD⁺ and glutathione — both synthesized primarily in the liver — reduce the organ’s capacity to regenerate and maintain redox balance [22] [23].
In essence: the hormonal chaos of perimenopause meets the natural slow down of the body’s detox machinery.
That’s why many womenexperience their first noticeable “aging acceleration” not because of age itself, but because of a mismatch between hormonal demand and metabolic capacity.
The Hidden Compounding Factor — Modern Life
Modern life quietly stacks the deck against the liver and gut.
Chronic stress elevates cortisol, which competes for the same detox pathways used to metabolize estrogen and progesterone [24].
Alcohol, sugar, and processed fats further deplete antioxidants and increase liver inflammation.
Lack of sleep and nutrient deficiencies impair glutathione and NAD⁺ regeneration, which are essential for both liver repair and hormonal detoxification.
In your 20s or early30s, your body’s resilience could compensate. But in your 40s — with antioxidant production declining and hormonal demands increasing — these stressors become visible: the dullness in your skin, the stubborn bloating, the irritability that wasn’t there before, the deep fatigue that no amount of coffee can fix.
The Gut Connection
The gut microbiome —particularly the estrobolome, a collection of bacteria that metabolize estrogen— becomes an equally crucial player [25].
When these bacteria are imbalanced due to antibiotics, chronic stress, or a low-fiber diet, estrogen is reabsorbed instead of eliminated, re-entering circulation and amplifying symptoms of estrogen dominance.
This internal feedback loop — liver overload, gut dysbiosis, hormonal recycling — explains why perimenopausal symptoms can appear “out of nowhere.”
It’s not random; it’s the body’s way of signaling that detoxification and hormone metabolism are falling out of sync.
Connecting the Dots
Perimenopause, then, isn’t simply a story of declining estrogen. It’s a systemic recalibration of metabolism, detoxification, and hormonal clearance.
When the liver is overloaded and the gut microbiome imbalanced, the hormonal rhythm falters — an devery system downstream feels it: mood, metabolism, sleep, skin, and weight.
Supporting these two systems — through targeted nutrition, stress balance, and antioxidant renewal —is one of the most effective ways to sustain hormonal harmony and cellularvitality throughout the perimenopausal years.
It’s not about resisting age — it’s about realigning with your biology.
BeMediq Preventive Insight
Emerging research confirms that perimenopause involves dynamic changes in estrogen and progesterone metabolism that stress hepatic detox pathways. Supporting the liver–gut axis helps reduce oxidative load, improves hormone clearance, and restores balance to the body’s natural rhythm.
How to Support Your Body Before Symptoms Start — A Smarter Way to Navigate Perimenopause
Understanding the why behind your symptoms is the first step — but the real transformation begins when you support the body that carries you through it.
The liver, your quiet multitasker, doesn’t just process hormones; it depends on steady fuel: nutrients, antioxidants, and rest.
After 40, its workload rises just as its own reserves begin to decline — making conscious nourishment not optional, but essential.
The good news?
You can lighten that load.
Science shows that certain foods, micronutrients, and targeted compounds can replenish hepatic antioxidants like glutathione and NAD⁺, stabilize hormone metabolism, and restore the body’s natural rhythm.
These molecules act as the liver’s biochemical currency:
Glutathione neutralizes free radicals and supports Phase II detoxification — crucial for estrogen and cortisol metabolism — while
NAD⁺ fuels the mitochondrial enzymes that drive cellular repair and energy production.
For some women, especially during perimenopause, lifestyle measures alone may not fully restore these pathways.
That’s where medical-grade supplementation — such as NAD⁺ injections or Glutathione nasal or injectable formulations — may offer additional support.
These delivery methods bypass the digestive system and directly elevate intracellular levels, helping the liver recover its rhythm and enhance hormonal clearance. (Always under professional guidance.)
This isn’t about“ detoxing” in the trendy sense — no green-juice cleanses or fasting fads. It’s about giving your body back its natural capacity to restore, renew, and rebalance.
How to Support Your Body Before Symptoms Start — A Smarter Way to Navigate Perimenopause
Continue reading:[The Liver-Hormone Connection — A Natural Way to Reduce Perimenopause Symptoms( Part III)]
FAQ — The Liver–Hormone Connection & Perimenopause
1. What exactly happens to hormones during perimenopause?
Perimenopause marks a gradual shift in ovarian function. Estrogen and progesterone start to fluctuate — sometimes rising sharply, sometimes dropping — while the body’s ability to clear hormones through the liver slows down. These changes can affect mood, metabolism, and overall energy.
2. Why is the liver so important for hormonal balance?
The liver metabolizes and deactivates estrogen, progesterone, cortisol, and other hormones after they’ve done their job. If this process becomes sluggish due to stress, diet, or nutrient depletion, hormonal signals can linger and amplify symptoms such as bloating, breast tenderness, or mood swings.
3. Can I improve hormonal balance just by “detoxing”?
Not exactly. Quick cleanses or extreme detox programs are rarely effective long-term. True hormonal detoxification happens daily through the liver’s natural enzyme systems — supported by nutrients like B vitamins, glutathione, and antioxidants, as well as consistent sleep and hydration.
4. What are early signs that my liver might be struggling with hormone clearance?
You may notice stronger PMS, heavier periods, water retention, fatigue, or irritability. These are not necessarily signs of disease — but they can indicate that your body’s detox pathways are under stress.
5. How do NAD⁺ and Glutathione support this process?
Both molecules are produced primarily in the liver and act as cellular protectors. NAD⁺ supports mitochondrial energy production and DNA repair, while glutathione neutralizes free radicals and helps transform hormones into water-soluble compounds for elimination.
6. Are NAD⁺ or Glutathione supplements safe for women in perimenopause?
Medical-grade formulations may support liver and metabolic health when used under professional guidance. They are not a replacement for hormones or medical therapy but may complement a balanced lifestyle and preventive strategy.
Disclaimer: These statements are for informational purposes only and have not been evaluated by the Food and Drug Administration. This content is not intended to diagnose,treat, cure, or prevent any disease. Always consult a licensed healthcare provider before starting any supplement or therapy.

Written by Elena Brull, FNR, Functional Nutrition Researcher & Women’s Health Journalist
About the Author
Elena Brull, FNR, is a Functional Nutrition Researcher and Women’s Health Journalist specializing in integrative approaches to hormonal balance, nutrition, and longevity. Her work combines evidence-based insights with holistic health principles to help women understand their biology and live in rhythm with it. She writes from a non-clinical, educational perspective — with the intention to inform and empower, not to diagnose or prescribe.
References:
[1]Braidy N, et al. Age-related changes in NAD⁺ metabolism oxidative stress and sirtuin activity in wistar rats. PLoS One.2011;6(4):e19194. [PMID: 21541336]
[2]Yoshida Y, et al. Age-related decreases in glutathione and its metabolic enzymes in human liver. J Gerontol A Biol Sci Med Sci. 2013;68(4):377–384.[PMID: 22904001]
[3]Katsyuba E, Auwerx J. Modulating NAD⁺ metabolism, from bench to bedside. EMBO J. 2017;36(18):2670–2683. [PMID: 28835536]
[4]Lu SC. Glutathione synthesis. Biochim Biophys Acta.2013;1830(5):3143–3153. [PMID: 22995213]
[5]Cichoż-Lach H, Michalak A. Oxidative stress as a crucial factor in liver diseases. World J Gastroenterol. 2014;20(25):8082–8091.[PMID: 25009380]
[6]García-Rodríguez JL, et al. Liver metabolism and regeneration: The role of redox homeostasis and NAD⁺. Int J Mol Sci.2020;21(9):3015. [PMID: 32375142]
[7]Marí M, et al. Mitochondrial glutathione: features, regulation and role in disease. Biochim Biophys Acta. 2013;1830(5):3317–3328. [PMID:23270890]
[8] López-Otín C, et al. The hallmarks of aging. Cell.2013;153(6):1194–1217. [PMID:23746838]
[9]Lee AJ, et al. Characterization of estrogen metabolism in human liver microsomes: involvement of CYP3A and CYP1A2. J Endocrinol.2003;179(3):239–247. [PMID: 14656212]
[10]Plášek J, et al. Hepatic metabolism of steroid hormones and its clinical implications. Physiol Res. 2022;71(S1):S57–S70. [PMID:35049556]
[11]Hristov BD. The role of glutathione metabolism in chronic illness development and its potential use as a novel therapeutic target. Cureus.2022;14(10):e29967. [PMCID: PMC9616098]
[12]Ballatori N, et al. Glutathione and the liver. Compr Physiol.2013;3(2):789–811. [PMID: 23720336]
[13]Prior JC. Perimenopause: The complex endocrinology of the menopausal transition. Endocr Rev. 1998;19(4):397–428. [PMID: 9715373]
[14]Santoro N, et al. Reproductive aging and the perimenopausal transition. Fertil Steril. 2021;115(4):1043–1050. [PMID: 33781602]
[15] Hale GE, RobertsonDM, Burger HG. The perimenopausal woman: Endocrinology and management. J Steroid Biochem Mol Biol. 2014;142:121–131. [PMID: 23911810]
[16]Randolph JF Jr, et al. The STRAW+10 criteria for reproductive aging: Menstrual cycle and hormonal changes. Menopause. 2011;18(11):1150–1156.[PMID: 21926851]
[17]Burger HG. The endocrinology of menopause. J Steroid BiochemMol Biol. 2011;118(4–5):257–260. [PMID: 21093904]
[18]Davis SR, et al. Understanding the menopause transition from a hormonal perspective. Lancet Diabetes Endocrinol. 2015;3(10):856–866. [PMID:26275339]
[19]Stefanska A, Bergmann K, Sypniewska G. Metabolic syndrome and menopause: Pathophysiology and management. Clin Chim Acta. 2015;438:60–64.[PMID: 25456806]
[20]Lu SC. Glutathione synthesis. Biochim Biophys Acta.2013;1830(5):3143–3153. [PMID: 22995213]
[21]Braidy N, et al. Age-related changes in NAD⁺ metabolism oxidative stress and sirtuin activity. PLoS One. 2011;6(4):e19194. [PMID:21541336]
[22]García-Rodríguez JL, et al. Liver metabolism and regeneration:The role of redox homeostasis and NAD⁺. Int J Mol Sci. 2020;21(9):3015. [PMID:32375142]
[23]Yoshida Y, et al. Age-related decreases in glutathione and metabolic enzymes in human liver. J Gerontol A Biol Sci Med Sci.2013;68(4):377–384. [PMID: 22904001]
[24]Vogel S, et al. Cortisol metabolism and liver function: The stress–detox axis. Endocr Rev. 2016;37(2):176–194. [PMID: 26518384]
[25] Baker JM, Al-NakkashL, Herbst-Kralovetz MM. Estrogen–gut microbiome axis: physiological and clinical implications. Maturitas.2017;103:45–53. [PMID: 28687293]