What’s happening to your body — and how to find your rhythm again.

When Everything Starts to Feel… Different
It begins quietly.
Maybe your periods change a little — heavier, or closer together.
Maybe your sleep feels fragile, or you wake up restless at 3 a.m. for no clear reason.
You notice you’re quicker to react, thinner in patience, easier to tears.
Your partner says, “You’ve been different lately,” and you wonder, am I?
Then come the headaches before your period — almost migraine-like.
Your skin feels drier.
Your hair, somehow, less alive.
You think: It must be stress. Or PMS.
But it’s something deeper — your hormones are beginning to shift.
Most women aren’t warned.
No one tells us that perimenopause — the long runway toward menopause —
can sometimes begin earlier than expected — most often in the forties, sometimes a little sooner in the late thirties, and usually unfolding gradually over several years before menopause, which on average arrives around age fifty-one.
It isn’t a sudden drop, but a slow rewiring of the hormonal systems that once kept us effortlessly balanced.
If only we knew earlier, we could meet these changes differently —
with nutrition that supports the liver and hormones,
with gentle botanical allies,
with rest instead of resistance,
with moments of honest inward reflection,
and with regular hormone check-ups — to see whether key hormones, especially progesterone, thyroid, and estrogen, are in balance, and to make timely adjustments that help the body find stability again under clinical guidance.
Understanding the Transition
Perimenopause refers to the years leading up to your final period, when estrogen and progesterone — the twin anchors of your reproductive rhythm — start to change their natural pattern.
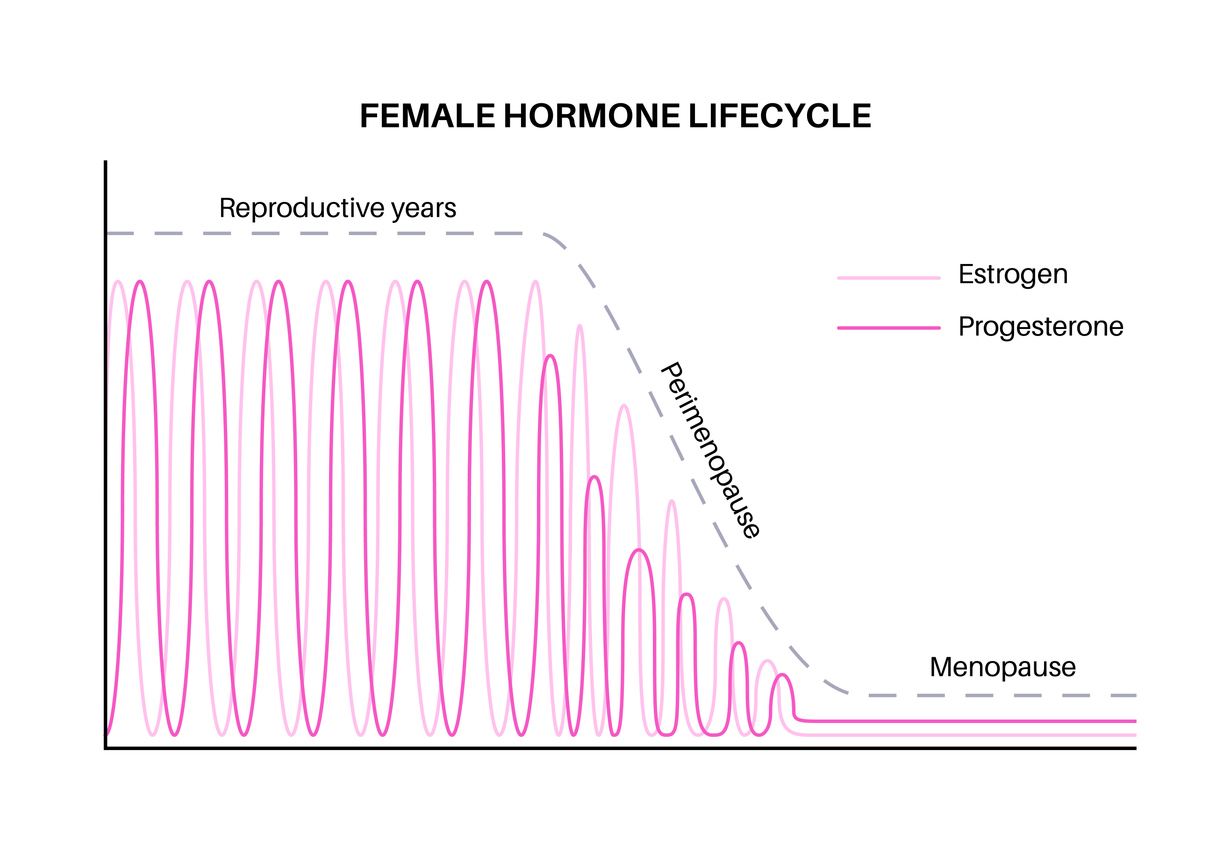
- Estrogen, once steady and cyclical, begins to rise and fall in uneven waves. Some months it soars too high, leaving you feeling irritable, bloated, or overstimulated. Other months it dips too low, and you might feel flat, unmotivated, or fatigued.
- Progesterone, which normally balances estrogen and promotes calm, begins to decline earlier and more consistently — especially when ovulation becomes irregular. That’s why you might sleep lightly or feel wired at night even when you’re exhausted.
Over time, the cycle becomes less predictable.
Some women notice shorter cycles — twenty-six instead of thirty days — while others experience long gaps or skipped periods. This irregularity signals that ovulation is becoming sporadic — the hall mark of the later perimenopausal stages.
For most, this transition feels like a conversation between body and self: subtle at first, then louder.
Each woman’s rhythm is unique. Understanding that these changes are not sudden or abnormal — but a gradual recalibration — turns anxiety into awareness.
What’s Happening in Your Hormones
Imagine your hormones as an orchestra that has played the same piece flawlessly for decades.
Each instrument — estrogen, progesterone, testosterone — knows its cue, its tempo, its tone.
And then, somewhere in your late 30s or early 40s, one section starts to lose sync.
The melody isn’t gone — it’s just… changing.
This is perimenopause: a time when your hormonal rhythm shifts from reproduction to renewal.
It’s not a collapse — it’s a recalibration.
Estrogen — The Vital Spark
Estrogen is your most expressive hormone.
It builds up the uterine lining, yes — but it also nourishes far beyond reproduction.
It keeps your brain sharp, your skin supple, your joints smooth, your heart resilient.
During perimenopause, estrogen doesn’t simply decline — it fluctuates wildly.
One cycle it’s too high, the next it drops overnight.
This rollercoaster explains why your mood, temperature, and energy can change within hours.
When estrogen soars, you might feel energized but edgy — a little overstimulated, prone to bloating or irritability.
When it drops, you might feel flat, foggy, or easily chilled, your skin drier, your motivation dimmer.
These fluctuations are guided by the hypothalamic-pituitary-ovarian axis, which gradually loses synchrony with age.
This ebb and flow isn’t chaos — it’s communication.
Your ovaries and brain are renegotiating how to maintain equilibrium after years of seamless coordination.
Progesterone — The Quiet Keeper of Calm
If estrogen is the melody, progesterone is the rhythm section — steady, grounding, soothing.
It’s produced after ovulation, and its job is to bring calm, balance, and deep sleep.
But as ovulation becomes less consistent, progesterone starts to fade first.
Without it, estrogen has no counter balance.
That’s why, even when estrogen levels are normal, you may feel:
- Restless at night, even when you’re tired
- More sensitive to conflict, noise, or caffeine
- Easily overheated or prone to headaches before your period
- Tearful, impatient, or “not like yourself”
It’s not in your head — it’s in your hormones.
Progesterone is what once softened life’s edges.
And as it diminishes, you may feel everything more intensely.
In early perimenopause, this decline often precedes significant changes in estrogen, explaining why sleep and anxiety symptoms can arise years before the final period.
The good news? There are ways to recreate that calm — naturally, nutritionally, or, when needed, therapeutically.
Testosterone — The Forgotten Flame
Often overlooked, testosterone continues to play a quiet but crucial role in your 40s and 50s.
It fuels motivation, focus, and desire, helps preserve muscle tone, and supports your mood.
As estrogen and progesterone fluctuate, testosterone’s relative influence shifts too.
You may feel more driven some months, then suddenly flat — not depressed, just disconnected from your spark.
Healthy testosterone balance doesn’t mean more aggression or libido; it means a sense of inner vitality — the confidence and strength that come from feeling capable and awake inside your own body.
There are currently no FDA-approved testosterone formulations specifically for women; if prescribed, they are used off-label in low, individualized doses under clinician supervision.
What Happens in Perimenopause — The Ripple Effects on Brain, Skin, and Metabolism
Hormones don’t act in isolation; they are messengers connecting every system in the body.
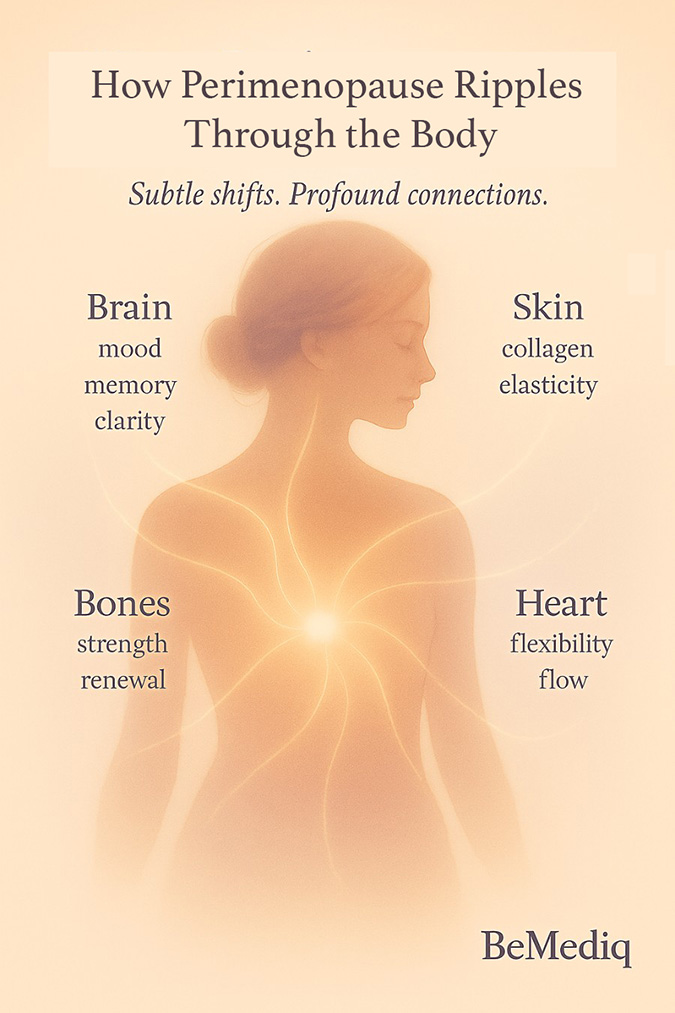
As estrogen and progesterone fluctuate, the ripple touches everything:
- The Brain — Estrogen supports serotonin and dopamine, the chemistry of optimism, focus, and flow. That’s why dips can bring fog, anxiety, or a sense that you’re “losing yourself,” even when you’re not.
- Muscles and Metabolism — Lower estrogen can make it harder to build or maintain muscle.
- Insulin sensitivity shifts, and fat storage — especially around the abdomen — can increase. This redistribution is linked to changes in estrogen-dependent insulin signaling and declining muscle mass rather than a sudden metabolic slowdown.
- Skin and Hair — Collagen renewal slows, moisture evaporates faster, and hair may thin slightly.
These are not vanity issues — they are visible reflections of the inner hormonal symphony changing key.
Treatment Options Explained
Once you understand what’s really happening, the next question almost always follows:
“So what can I do?”
And that’s where most women get lost — in a maze of supplements, miracle promises, and fear-based messages about “aging.”
But the truth is quieter.
You don’t need to fight your body.
You need to work with it — nourish it, listen to it, and give it what it’s been giving you all along: patience and care.
This stage isn’t about fixing something broken.
It’s about supporting the systems that are trying to find a new balance.
Start with the Foundations
Before any prescription or protocol, there are three pillars that define how gracefully your body adapts:
- how you eat,
- how you move,
- and how you rest.
Nutrition – feeding your hormones
Your hormones are built from nutrients — amino acids, healthy fats, and minerals — and rely on vitamins and steady energy from complex carbohydrates to keep their production in balance.
When estrogen and progesterone begin to fluctuate, your body doesn’t need restriction — it needs nourishment that keeps blood sugar, mood, and energy steady.
Balanced blood sugar is the foundation of hormonal calm.
Meals that combine slow-digesting carbohydrates, protein, healthy fats, and fiber help maintain that stability naturally.
Each meal is an opportunity to restore balance — to give your body the raw materials it needs to create harmony from within.
- Protein can come from legumes, whole grains, or dairy-based sources, providing the amino acids needed for hormone synthesis and tissue renewal.
- Good fats — from avocado, olive oil, nuts, and seeds — offer the building blocks for steady hormone production.
- Fiber-rich foods — like vegetables, whole grains, legumes and fruits — help stabilize blood sugar by slowing glucose absorption and improving insulin sensitivity.
- And cruciferous vegetables such as broccoli, kale, and cauliflower assist your liver in clearing excess estrogen. The liver itself is one of the most underestimated keys to hormonal harmony during the transition. If you’d like to understand this connection more deeply — how liver health and hormonal balance are two sides of the same system — explore our feature “The Liver–Hormone Connection: A Natural Way to Reduce Perimenopause Symptoms"
- For extra support, nutrients like glycine, NAC, or taurine can gently assist detox and energy pathways — especially for women following plant-forward diets.
Explore our article "BeMediq Scientific Spotlight: The Importance of Nutrition in Menopause and Perimenopause" to learn how nutrition influences the menopause transition.
Coming Soon — Your Everyday Guide: (For practical recipes, meal ideas, and a full seven-day plan inspired by science, see the upcoming BeMediq eBook — “Nutrition for Women in Perimenopause and Beyond.”)
*These nutritional strategies are supportive but not curative; they complement clinical care and are not substitutes for hormone therapy when medically indicated.
Movement – building strength and flow

In perimenopause, exercise is no longer optional — it’s obligatory.
Strength training preserves muscle and stabilizes insulin sensitivity.
Walking, yoga, and stretching calm the nervous system that progesterone once steadied.
You don’t need intensity; you need consistency.
Sleep – the nightly repair cycle
Sleep used to happen naturally; now it must be courted.
Create evening rituals: magnesium, herbal tea, light stretching, journaling.
If night sweats wake you, cooling layers and stable blood sugar can make all the difference.
Sleep is not indulgence — it’s hormone therapy in disguise.
Non-Hormonal Support — Gentle First Steps
Sometimes, your body needs help finding its rhythm again before introducing hormones.
Certain nutrients and botanicals can help modulate the fluctuations that cause most discomforts.
Examples include:
- Magnesium glycinate* - to calm the nervous system
- B vitamins* - for energy and neurotransmitter balance
- Ashwagandha or Rhodiola* - adaptogens to ease stress-related cortisol spikes
- Omega-3s* – to reduce inflammation and support mood stability
- MIC-B12* - combines Methionine, Inositol, Choline, and Vitamin B12, nutrients that may support metabolic health, liver function, and energy production.
- NAD⁺support* - may help promote healthy cellular energy and mitochondrial function.
- Glutathione* - a key antioxidant that may help protect cells from oxidative stress and support natural detoxification processes.
*All supplement statements describe general structure/function support and are not intended to diagnose, treat, cure, or prevent disease, in accordance with FDA and FTC guidelines.
Hormone Replacement Therapy (HRT) — Modern, Bioidentical, Balanced

For some women, the fluctuations run too deep for lifestyle alone to steady.
That’s where HRT — bioidentical hormone therapy — can bring the body back into balance.
The word “hormone therapy” can sound intimidating, but it simply means replacing what’s missing in a form your body recognizes.
Bioidentical hormones are molecularly identical to what your body produces — so they bind to receptors naturally and predictably.
There are several forms, each with its rhythm and personality.
Want to understand HRT Options? Read: "Understanding HRT Options – Gel vs. Patch vs. Tablets"
Bioidentical vs. Synthetic — What’s the Difference?
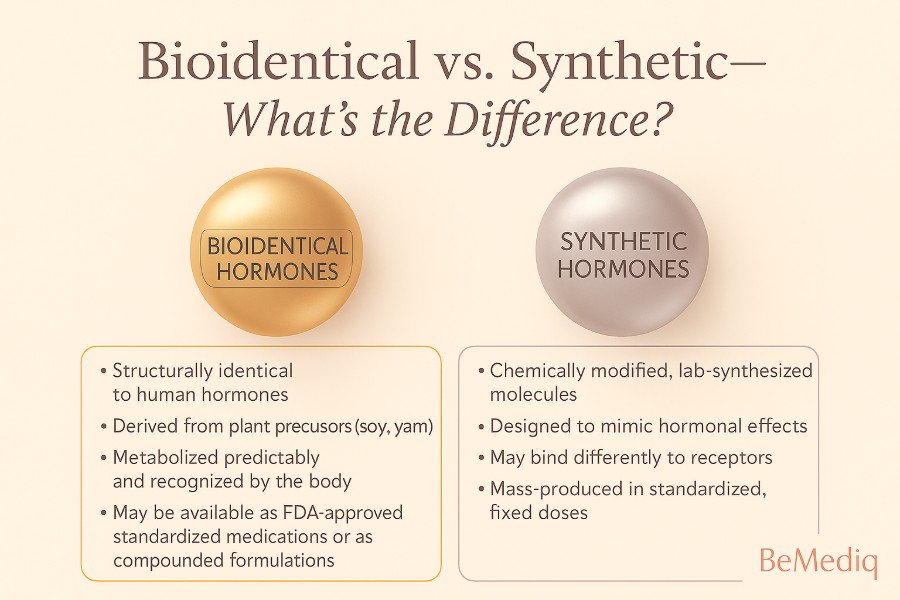
Synthetic hormones,
historically used in older therapies, are chemically altered and can behave differently in the body.
Bioidentical hormones,
in contrast, are derived from plant sources and structurally identical to human hormones.
They are compounded in precise, personalized doses — allowing for a gentler, more adaptive approach.
BeMediq uses clinician-guided compounding through licensed 503A pharmacies, ensuring pharmaceutical quality with human sensitivity.
Discover Personalized Hormone Therapy
Curious about bioidentical hormones? Explore our article: "Compounded vs. FDA-Approved Bioidentical HRT: Understanding the Difference"
Dispelling the HRT-Myth
There’s still confusion around HRT — much of it based on outdated studies.
Modern bioidentical hormone therapy is far safer and more nuanced than older synthetic regimens.
The North American Menopause Society (NAMS, 2022) and ACOG now recognize that for healthy women under 60 — particularly within 10 years of menopause — HRT may offer protective effects for bone, heart, and cognitive health, beyond symptom relief.
However, HRT is not prescribed to prevent heart disease or dementia; its primary indication remains the relief of vasomotor and genitourinary symptoms, and the prevention of bone loss.
Hormone therapy isn’t a one-way street — it’s a guided journey with checkpoints, clinical care, and balance.
Is HRT Right for You?
How to know when your body is asking for more than lifestyle alone.
Every woman reaches a point where she starts to wonder:
Is this still normal — or am I missing something my body needs?
Maybe you’ve done everything right.
You’ve cleaned up your diet, you move, you meditate, you sleep as best you can— and yet, something still feels off.
You’re exhausted but wired.
Your skin doesn’t respond to care like it used to.
You can’t focus the way you once did.
You still recognize yourself — but it’s a fainter version.
That’s often the moment when the question arises:
Would hormone therapy help?
The Turning Point: When Symptoms Outweigh Adaptation
Perimenopause asks a lot of your body — it demands constant adaptation.
But when that adaptation begins to cost too much — when the sleep loss, mood swings, or exhaustion start eroding your quality of life — it may be time to consider additional support.
Hormone therapy isn’t about reversing age or fixing you.
It’s about restoring the internal conversation that became too quiet.
Your BeMediq clinician will help you identify whether your symptoms reflect simple fluctuation or a true deficiency that needs replenishment.
When HRT May Be Worth Considering
You don’t need to check every box, but if you recognize yourself in several of these, it may be worth exploring:
- Sleep has become light, broken, or anxious — and no routine helps.
- You wake with night sweats or a racing mind.
- Your skin feels thinner, your hair less full, your glow dimmer.
- You notice brain fog, loss of motivation, or emotional flatness.
- You’ve lost strength or muscle tone despite regular movement.
- Sex feels uncomfortable — or your desire feels distant.
- You’ve gained weight around your waist, even with the same habits.
These aren’t failures. They’re biological feedback from a body whose hormones have changed pace.
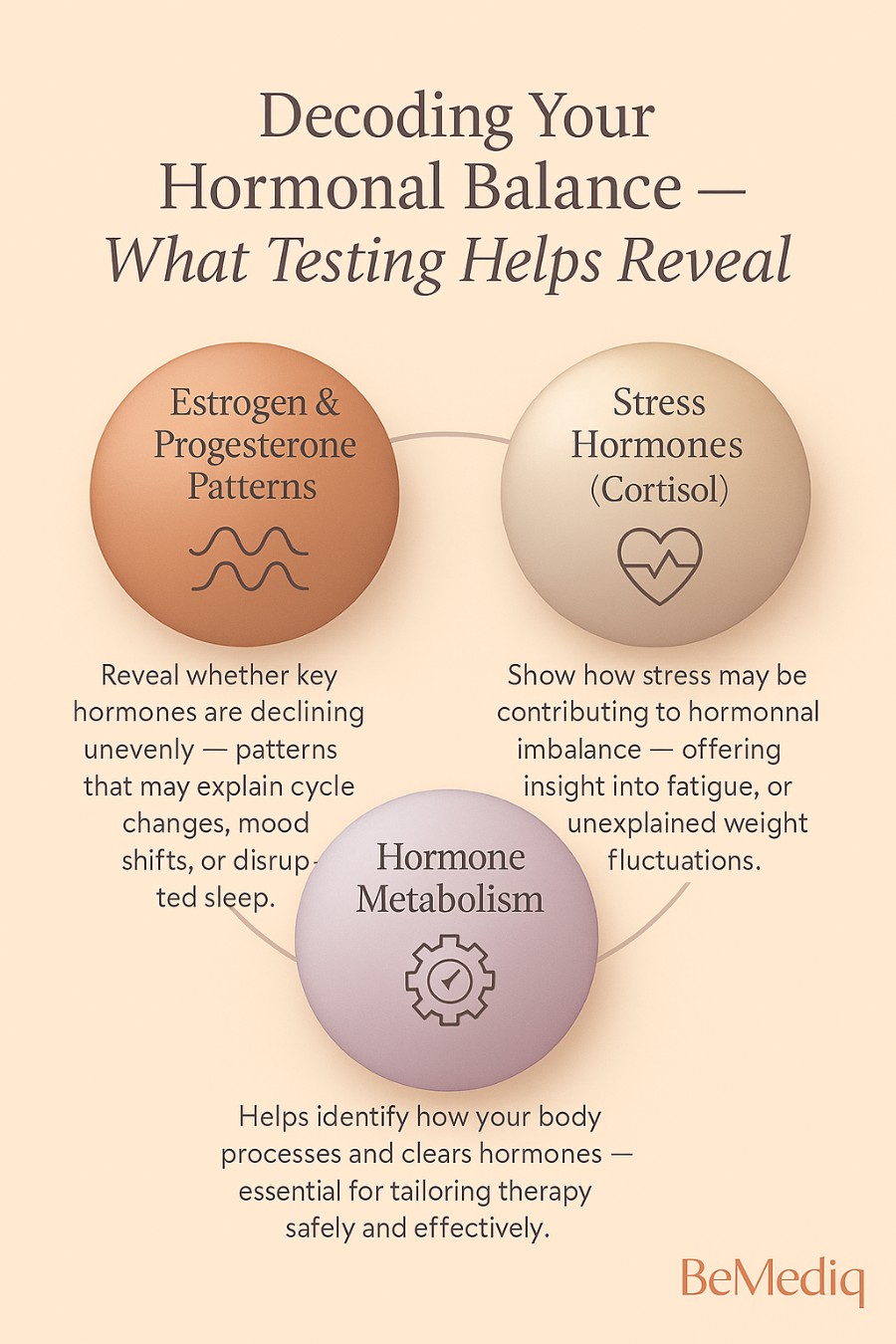
The Power of Knowing — Why Testing Matters Before HRT
At some point, awareness turns into curiosity.
You’ve noticed the shifts — in sleep, mood, or how your body responds — but what you really want now is to understand them. That’s where testing becomes more than data; it becomes self-knowledge.
Comprehensive hormone testing reveals what’s happening beneath the surface — whether estrogen and progesterone are fluctuating unevenly, whether thyroid or HPA-axis patterns are adding to the fatigue, or whether insulin resistance might be quietly influencing your energy and weight.
Regular testing isn’t only about diagnosis — it supports risk assessment and early discussion of prevention.
When relative estrogen dominance persists for years, it may influence how cells grow and renew — and studies have observed associations between long-term imbalance and certain hormone-sensitive conditions, including those affecting breast or uterine tissue.
And when DHT or testosterone run high, you may notice clues that seem disconnected — changes in skin, thinning hair, or that stubborn belly weight that defies your usual habits.
The truth is, similar symptoms can mask very different root causes.
Low thyroid function, HPA-axis dysregulation, PCOS, or blood-sugar imbalance can all echo the hormonal shifts of perimenopause.
That’s why no woman should start hormone therapy based on symptoms alone.
Testing brings the story into focus.
It allows your clinician to support your unique biology — precisely, safely, and effectively.
Because knowing your numbers isn’t about chasing perfection; it’s about understanding your body’s rhythm, and working with it.
According to the North American Menopause Society (NAMS) and the American College of Obstetricians and Gynecologists (ACOG), routine hormone testing is not required to diagnose perimenopause — which is primarily a clinical diagnosis.
However, targeted laboratory evaluation can help rule out overlapping conditions (such as thyroid or adrenal dysfunction) and individualize treatment when hormone therapy is considered.
BeMediq’s at-home hormone panels measure estrogen, progesterone, LH, FSH, testosterone, thyroid, and cortisol — the key markers that help decode your current phase and guide next steps with clarity and confidence.
At BeMediq, we begin every plan with clarity.
Through at-home hormone testing, your clinician sees where you truly stand —not just in numbers, but in patterns.
Explore At-Home Testing
For educational purposes only. Not intended to diagnose, treat, or replace professional medical advice.
Testing helps identify:
- Whether estrogen or progesterone are declining unevenly
- If stress hormones (like cortisol) are adding to the imbalance
- How your body metabolizes hormones — key for safety and efficacy
Because hormone levels can fluctuate significantly — especially during perimenopause — they should never be interpreted in isolation. Your clinician considers your symptoms, cycle timing, and overall health history to understand what the numbers truly mean and how they fit into your broader hormonal picture.
Reclaiming Balance
Menopause is not the end of youth — it’s the evolution of wisdom.
There comes a moment — often quietly, often late at night — when you realize you’ve crossed into something new.
Your body feels different, yes.
But so do you.
For years, you’ve moved through the world guided by hormones that once dictated every rhythm — every surge of energy, every mood, every cycle of creation and release.
Now, that rhythm is softening.
And for the first time, it’s not about fertility, productivity, or perfection —it’s about balance.
The Reality Check — What to Know Before You Begin HRT
Before starting hormone therapy, most women have the same unspoken questions:
Will this truly help me regain that inner equilibrium — the calm energy and confidence I used to move through life with? Will it help me maintain my curves, my waistline, my skin and hair — the quiet signatures of my femininity?
These are not superficial questions.
They reflect a deep wish to stay vital, balanced, and connected to one’s sense of womanhood — all of which are profoundly influenced by hormones.
HRT may help restore what fluctuating estrogen and progesterone once supported — smoother skin, steadier mood, better sleep, improved muscle tone, and a more youthful fat distribution. But it’s not a cosmetic shortcut; it’s a clinical therapy that replenishes hormones your body naturally produced for decades.
Still, discernment matters.
Some doctors remain cautious, often citing outdated studies that linked older synthetic regimens to higher cancer risks.
Yet modern research — including position statements from the North American Menopause Society (NAMS, 2022) and the American College of Obstetricians and Gynecologists (ACOG, 2023) — shows that bioidentical or body-identical hormone therapy, when prescribed under medical supervision, is considered safe for healthy women under 60 or within 10 years of menopause, provided it’s individualized and monitored.
Every woman’s response, however, is unique.
Some notice benefits within weeks; others need gradual adjustments.
Occasionally, early side effects such as breast tenderness or mild mood changes appear, but they usually settle as equilibrium returns.
And what if you stop?
Discontinuing HRT doesn’t accelerate aging; it simply allows the body to return to its natural baseline.
This is why therapy should begin only with clear clinical indication — and always be tapered thoughtfully under a clinician’s guidance.
Perimenopause is an emotional chapter not because of the treatment decision, but because the brain itself is undergoing neurological adaptation — a rewiring process influenced by changing estrogen and progesterone patterns.
Hormone therapy should never be an impulsive or emotional choice.
It’s an informed, evidence-guided step made with your clinician, based on your body’s unique needs.
Postmenopause — The Still Point After the Storm
Once your hormones stabilize into postmenopause, the noise begins to fade.
The hot flashes lessen, the sleep slowly returns.
Your body finds a quieter pulse — one that no longer changes every month, but sustains every day.
This is the moment to rebuild, not chase.
- To give your body the nutrients it was once too busy to store.
- To strengthen muscles that now define your shape and protect your bones.
- To feed your mind the calm it has long been craving.
With the right support — lifestyle, nutrients, and sometimes HRT — this phase can become the most grounded, radiant chapter of your life.
Keep in mind: continuing HRT is a personal choice; ongoing evaluation every 6–12 months ensures benefits still outweigh risks.
The New Landscape of Vitality
Science now understands what women have long known intuitively:
estrogen and progesterone don’t just regulate cycles — they influence the brain, skin, heart, and emotions.
When supported wisely, these hormones can continue to serve your health and beauty far beyond the reproductive years.
What changes is the intention.
You’re no longer sustaining the possibility of new life — you’re sustaining your own.
This stage is not a decline.
It’s a refinement — a shift from doing to being, from output to embodiment.
Emotional Balance — The Inner Hormone
As your body’s chemistry stabilizes, your emotional landscape begins to reshape, too.
There’s often a new clarity — not because life gets easier, but because you do.
You start saying "no" with ease.
You start sleeping through the noise, literally and figuratively.
You stop proving, and start choosing.
This emotional steadiness isn’t accidental — it’s biological grace.
When estrogen fluctuations calm, the nervous system steadies, cortisol eases,and you regain the centeredness you thought was lost.
It’s the quiet power of a woman who knows herself — no longer swayed by cycles, but led by choice.
Good to know: Emotional well-being after menopause has been linked to improved sleep quality, stabilized cortisol rhythms, and greater parasympathetic resilience — effects often supported by lifestyle and, when indicated, low-dose hormone therapy.
The BeMediq Approach — Science with Sensibility
At BeMediq, we believe the transition into menopause is not a medical condition— it’s a natural evolution that deserves intelligent care.
Our role is to bridge science with empathy, guiding you through the options —from lifestyle to bioidentical hormones — so you can move forward with confidence, not confusion.
Through at-home testing, personalized care, and clinician-guided hormone support, we help you understand the story your body is telling — and how to honor it.
You don’t need to chase your old self.
You just need to meet the woman you’re becoming.
Personalization — The BeMediq Way
Sometimes it’s hard to find clarity in the noise. So much advice, so many promises — and yet, every woman’s story is different.
Your symptoms, your rhythm, your way of responding — they’re as individual as you are.
That’s when it becomes time to seek guidance from someone who understands the science — and you.
Your hormones don’t just need balance — they need understanding.
That’s why every BeMediq plan begins with:
- An online consultation with a licensed clinician
- At-home hormone testing for insight into your unique profile
- A personalized formulation, compounded and shipped discreetly to your door
Your plan evolves with you — because your hormones do too.
Explore At-Home Testing.
Find Your Ideal Hormone Plan.
Key Takeaways— The Complete Guide to Perimenopause & Menopause
Perimenopause is a transition, not a decline.
Perimenopause can begin in your late 30s or 40s and unfold gradually over several years before menopause. Hormones don’t shut down — they recalibrate.
Hormonal fluctuation is the hallmark — not absence.
Estrogen rises and falls unpredictably, while progesterone quietly declines first. This imbalance can cause sleep changes, mood swings, and anxiety long before your final period.
Your brain and body are adapting — not failing.
Shifts in estrogen and progesterone influence the hypothalamus, pituitary gland, and neurotransmitters such as serotonin and dopamine. These changes affect emotion, focus, and sleep but are part of a neurological adaptation process.
Every symptom tells a story.
Fatigue, hair loss, belly weight, or anxiety are not random — they reflect how your body responds to hormonal signals, metabolism, and stress pathways (like the HPA axis).
Lifestyle is the first therapy.
Nutrition, movement, and rest form the foundation of hormonal balance. Protein, healthy fats, and fiber stabilize blood sugar, while strength training and restorative sleep support metabolic and emotional stability.
The liver plays a silent but central role.
Liver function is essential for metabolizing hormones and maintaining equilibrium. Nutrients like choline, NAC, and glycine can support healthy detoxification and hormone clearance.
Hormone testing turns confusion into clarity.
Comprehensive hormone testing (estrogen, progesterone, testosterone, thyroid, cortisol, LH, FSH) helps distinguish perimenopause from thyroid, adrenal, or insulin imbalances. It ensures therapy decisions are evidence-based, not symptom-based.
HRT can be safe and effective — when personalized.
Modern bioidentical hormone therapy (estradiol, progesterone) mimics natural hormones and, under clinician guidance, may relieve symptoms and support bone, heart, and cognitive health for women under 60 or within 10 years of menopause.
Perimenopause is not just hormonal — it’s emotional and neurological.
Perimenopause affects identity, mood, and confidence because the brain is recalibrating its hormonal communication network. Support — clinical, emotional, and lifestyle — helps restore inner equilibrium.
Postmenopause is not the end.
Once hormones stabilize, energy, sleep, and mood often improve. With mindful nutrition, strength, and rest, this phase can become your most grounded and radiant chapter.
The BeMediq approach: Science with sensibility.
Menopause is not a medical failure but a biological evolution. Through at-home testing, personalized plans, and clinician-guided bioidentical therapy, BeMediq helps women navigate this transition with confidence, not confusion.
BeMediq — Where Science Meets Sensibility
FAQs — Understanding Perimenopause & Menopause
When does perimenopause usually begin?
It often starts in your early to mid-40s — sometimes earlier in the late 30s — and can last anywhere from 4 to 8 years before menopause. The average age of menopause (the final period) is around 51.
How do I know if what I’m feeling is perimenopause — or something else?
Common signs include cycle changes, sleep disturbances, mood swings, and new sensitivities to stress or temperature.
However, similar symptoms can stem from thyroid issues, adrenal fatigue, or insulin resistance — that’s why testing helps reveal the true cause.
What’s the difference between perimenopause and menopause?
Perimenopause is the transition phase leading up to menopause, marked by hormonal fluctuations and irregular periods.
Menopause itself is confirmed after 12 consecutive months without a period.
Can perimenopause affect mood and focus?
Yes. Changing estrogen levels influence neurotransmitters like serotonin and dopamine, which regulate mood, memory, and emotional stability. That’s why many women experience anxiety, brain fog, or emotional swings during this time.
Is hormone therapy (HRT) safe?
Modern bioidentical HRT — when prescribed and monitored by a clinician —is considered safe for healthy women under 60 or within 10 years of menopause.
Hormone therapy works best when it’s tailored — aligned with your biology, not generalized averages.
Regular follow-ups and dose adjustments ensure that treatment remains both effective and balanced over time.
Should I test my hormones before starting HRT?
Yes. While perimenopause is mainly a clinical diagnosis, targeted testing (estrogen, progesterone, thyroid, cortisol, testosterone) helps rule out overlapping conditions and ensures therapy is tailored to your biology.
Can lifestyle changes really make a difference?
Absolutely. Nutrition, movement, and sleep are foundational for hormonal harmony.
Balanced meals, liver-supportive foods, strength training, and stress management can ease many symptoms — even before considering HRT.
Disclaimer: These statements are for informational purposes only and have not been evaluated by the Food and Drug Administration. This content is not intended to diagnose,treat, cure, or prevent any disease. Always consult a licensed healthcare provider before starting any supplement or therapy.

Written by Elena Brull, FNR, Functional Nutrition Researcher & Women’s Health Journalist
About the Author
Elena Brull, FNR, is a Functional Nutrition Researcher and Women’s Health Journalist specializing in integrative approaches to hormonal balance, nutrition, and longevity. Her work combines evidence-based insights with holistic health principles to help women understand their biology and live in rhythm with it. She writes from a non-clinical, educational perspective — with the intention to inform and empower, not to diagnose or prescribe.
Citation:
Brull, Elena. The Complete Guide to Perimenopause & Menopause. BeMediq Scientific Spotlight, Oktober 2025. Available at: https://www.bemediq.com/blogs/the-complete-guide-to-perimenopause-menopause
References:
- Soules MR, et al. Executive summary of the Stages of Reproductive Aging Workshop + 10 (STRAW + 10). Menopause. 2012; 19(4): 387–395.
PMC3340903), DOI: 10.1097/gme.0b013e31824d8f40. - The North American Menopause Society. The 2022 Hormone Therapy Position Statement of The North American Menopause Society. Menopause. 2022; 29(7): 767–794. PMID: 35797481, DOI: 10.1097/GME.0000000000002028.
- Brinton RD. Estrogen regulation of the brain: therapeutic implications. Endocr Rev. 2009; 30(4): 407–410.
- Thornton MJ. Estrogens and skin aging. Dermatoendocrinol. 2013; 5(2): 264–270, PMCID: PMC 3772914 PMID: 24194966.
- Compston JE. Sex steroids and bone. Physiol Rev. 2001; 81(1): 419–447. PMID: 11152762, DOI: 10.1152/physrev.2001.81.1.419.
- Magraith, K., & Jang, C. (2023). Management of menopause. Australian Prescriber, 46(3), 48–53. DOI: https://doi.org/10.18773/austprescr.2023.014, PMCID: PMC10665088; PMID: 38053812.
- Giannini, A., Caretto, M., Genazzani, A. R., & Simoncini, T. (2021). Neuroendocrine Changes during Menopausal Transition. Endocrines, 2(4), 405–416. DOI: https://doi.org/10.3390/endocrines2040036.
- Prior JC. Perimenopause: the complex endocrinology of the menopausal transition. J Steroid Biochem Mol Biol. 2018; 182: 11–19. PMID: 9715373.
- Greendale, G. A., Sternfeld, B., Huang, M., Han, W., Karvonen-Gutierrez, C., Ruppert, K., Cauley, J. A., Finkelstein, J. S., Jiang, S.-F., & Karlamangla, A. S. (2019, 7. März). Changes in body composition and weight during the menopause transition. JCI Insight, 4(5), e124865. DOI: 10.1172/jci.insight.124865, PMCID: PMC6483504.
- North American Menopause Society (NAMS). Guideline: Laboratory Testing in Menopause Evaluation. Menopause. 2022 (Supplemental Section). PMID: 35797481, DOI: 10.1097/GME.0000000000002028.
- Erdélyi, A., Pálfi, E., Tűű, L., Nas, K., Szűcs, Z., Török, M., Jakab, A., & Várbíró, S. (2023, 21. Dezember). The Importance of Nutrition in Menopause and Perimenopause - A Review. Nutrients, 16(1), 27. PMCID: PMC10780928, PMID: 38201856.
- Baker, F. C., Lampio, L., Saaresranta, T., & Polo-Kantola, P. (2018). Sleep and sleep disorders in the menopausal transition.Sleep Medicine Clinics, 13(3), 443–456. , PMCID: PMC6092036 , PMID: 30098758, DOI: 10.1016/j.jsmc.2018.04.011.
- Stuenkel, C. A., Davis, S. R., Gompel, A., Lumsden, M. A., Murad, M. H., Pinkerton, J. V., & Santen, R. J. (2015). Treatment of symptoms of the menopause: An Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism, 100(11), 3975–4011. DOI: https://doi.org/10.1210/jc.2015-2236
- Yager JD, Davidson NE. Estrogen carcinogenesis in breast cancer. N Engl J Med.2006;354(3):270–282. DOI: 10.1056/NEJMra050776.
- Key TJ et al. Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst.2002;94(8):606–616. PMID: 11959894, DOI:10.1093/jnci/94.8.606
- Kaaks R et al. Sex hormones, insulin, IGF-I and risk of breastcancer. EndocrRelat Cancer. 2005;12(4):1071–1102. DOI:10.1677/erc.1.01014.
License:
© 2025 BeMediq.
This article is published under a Creative Commons Attribution–NonCommercial–NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
Educational sharing is permitted; commercial use or modification requires written permission from the author and BeMediq.