Based on a 2024 review in Antioxidants (Basel) by Tuell et al., "The Role of Glutathione and Its Precursors in Type 2 Diabetes" Spotted in PMC10885928

The Big Question
Diabetes is not only about blood sugar. It’s also about the silent storm of oxidative stress and mitochondrial dysfunction that damages cells over time. Glutathione (GSH), the body’s most powerful antioxidant, is consistently low in patients with type 2 diabetes. But can lifestyle and supplementation help restore it — and in doing so, slow disease progression?
This was the very question Tuell and colleagues set out to explore. In their 2024 review, they sifted through decades of experimental studies, clinical trials, and biochemical data to trace the connection between glutathione metabolism and type 2 diabetes. They asked:
- Why do patients lose glutathione?
- What are the molecular consequences? and
- Could interventions — from exercise and nutrition to precursor supplementation — tip the balance back toward resilience?
What the Scientists Found
When scientists dug deeper, they realized diabetes isn’t just a matter of “too much sugar.” It sets off a cascade, like dominoes tipping into each other.
First, glutathione levels drop. Chronically high glucose fuels a flood of free radicals, and over time patients are left with less of the reduced, protective form of GSH and more of the oxidized, exhausted kind — a red flag of cellular stress.

Glutathione works like the body’s shield against oxidative stress. This cycle shows how it is built, used to neutralize free radicals, and then recycled back into its active form. For educational purposes only. Not medical advice.
But the problem doesn’t stop there. Diabetes also weakens the body’s protective mechanisms. The very enzymes responsible for building and recycling glutathione — glutathione synthetase, γ-glutamylcysteine synthetase, glutathione peroxidase — begin to falter. Even when raw materials are present, the system works sluggishly, like an engine running on low oil.
And then comes the cruel loop. With too little glutathione, insulin signaling grows weaker. The body struggles to move sugar into cells. Blood sugar rises higher. More free radicals are produced. Which drains glutathione further. The cycle feeds itself, pulling the body deeper into oxidative stress.
Beyond Blood Sugar – The Complications
The danger of diabetes isn’t only written in numbers on a glucose meter. It’s written in the slow spread of oxidative stress, moving silently through the body.
Blood vessels lose their flexibility, paving the way for cardiovascular disease. Nerves, constantly bathed in free radicals, begin to misfire, leading to neuropathy and the gradual loss of sensation. The kidneys, forced to filter blood laced with oxidative byproducts, take on relentless strain, setting the stage for nephropathy. And in the eyes, tiny vessels weaken, light itself becoming clouded through retinopathy.
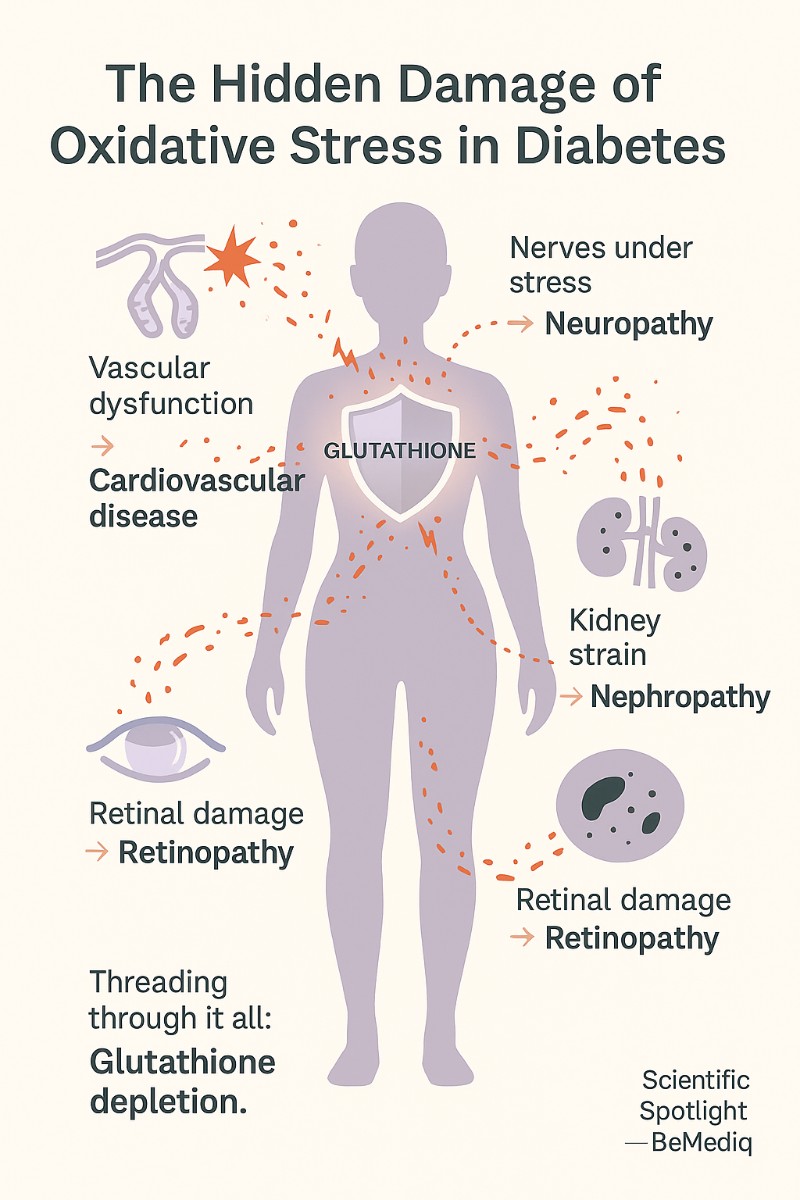
Oxidative stress doesn’t just raise blood sugar — it slowly damages blood vessels, nerves, kidneys, and eyes. When glutathione, the body’s protective shield, is depleted, tissues become vulnerable and complications of diabetes begin to appear. For educational purposes only. Not medical advice.
Threading through all of these complications is one quiet constant: glutathione depletion. Without its protection, tissues are left vulnerable, and the hidden damage of oxidative stress becomes the visible burden of chronic disease.
Lifestyle as Medicine
What Tuell and colleagues highlight is both reassuring and empowering: glutathione is not fixed. It can be shaped — and strengthened — by the choices we make every day.
When we move our bodies, muscles don’t just grow stronger; they also learn to produce more glutathione, training their antioxidant enzymes as if they were part of the workout. (Scientific Spotlight - Glutathione & Exercise: How Training Builds Your Inner Shield Against Aging) The food we choose adds another layer: meals rich in sulfur-containing amino acids, fresh vegetables, and antioxidant vitamins feed the recycling loops that keep GSH available. (Scientific Spotlight - How Can We Raise Glutathione Inside Cells?)
Even body weight matters. Carrying excess fat places a constant oxidative burden on cells, but finding balance in energy intake helps ease that hidden pressure at its source. And then there is rest: sleep and circadian rhythms, still only partly understood, appear to whisper instructions to the antioxidant system — a reminder that rhythm and recovery are as vital as movement and fuel.
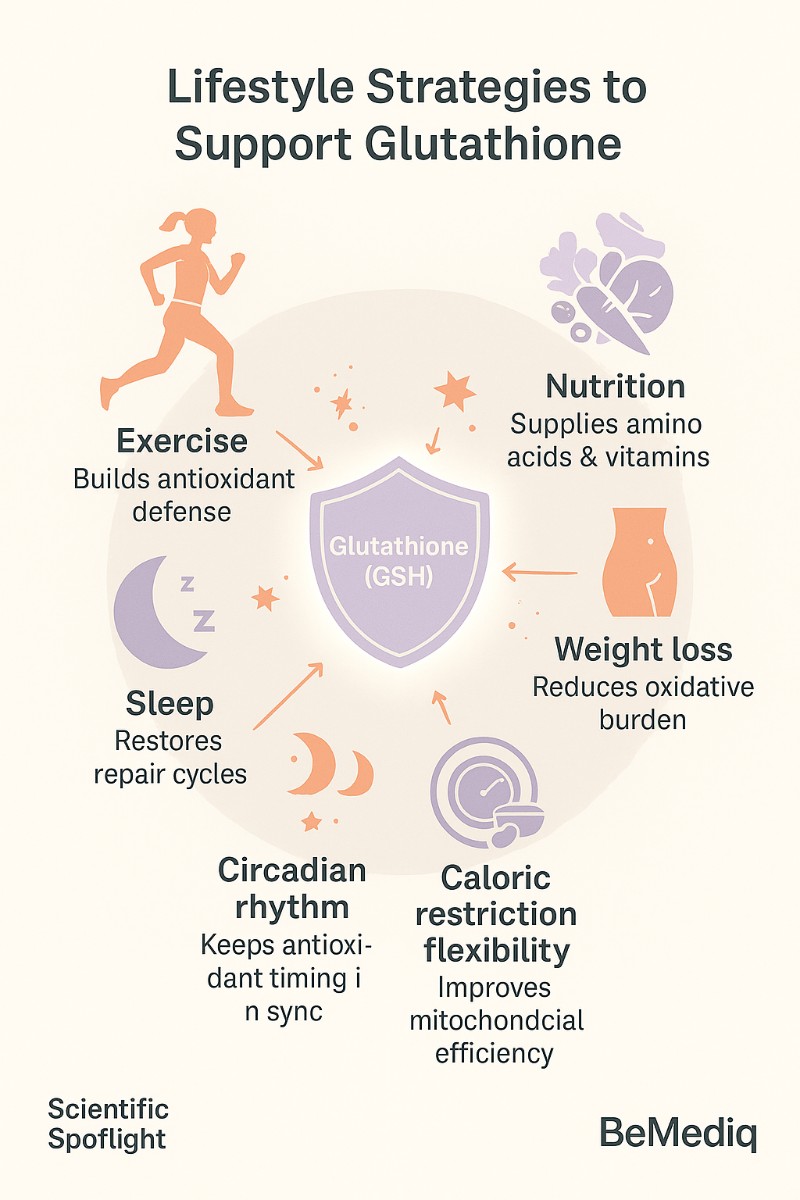
Lifestyle choices like exercise, good nutrition, healthy weight, restful sleep, and balanced rhythms may help the body protect and recycle glutathione. For educational purposes only. Not medical advice.
Each habit may seem small on its own. But together, they form a quiet architecture of resilience, helping the body rebuild the shield that diabetes so often erodes.
The Case for Supplementation
Lifestyle lays the foundation, but for many, the body still struggles to keep up with demand. Here the review turns to precursor support — nutrients that don’t replace glutathione, but help the body rebuild it from within.
One of these is N-acetylcysteine (NAC), a form of cysteine that replenishes the most limited ingredient in glutathione synthesis. On its own, it offers support. But when paired with glycine, the result is GlyNAC — a combination that has drawn increasing scientific attention.
In early trials, GlyNAC has done more than refill the antioxidant reservoir. It has been shown to restore glutathione pools, improve mitochondrial function, reduce markers of inflammation and oxidative stress, and even enhance insulin sensitivity.
The evidence is still young, and large clinical trials are needed before GlyNAC becomes standard care. Yet the direction is clear: supplementing the body’s own resilience may one day stand alongside exercise and nutrition as part of a comprehensive strategy against diabetes and its complications.
Modern Extensions: Can We Support Glutathione Even Further?
While Tuell et al. focus on precursor strategies, modern clinical practice has also begun exploring direct delivery methods.
- Glutathione injections provide the compound directly into the bloodstream, bypassing digestion.
- Nasal sprays may deliver GSH across mucosal membranes, offering another route for rapid uptake.
These methods are not evaluated in the review itself, but they represent a growing interest in how glutathione can be supported beyond lifestyle and precursors. For individuals under high oxidative stress — whether from diabetes, aging, or intense training — such approaches may offer an additional layer of resilience when guided by professional care.
Practical Wisdom
What Tuell and colleagues leave us with is more than data points — it is a roadmap for resilience.
We can train the system: every bout of movement teaches muscle to defend itself better, building glutathione as surely as it builds strength.
We can feed the system: meals rich in sulfur amino acids, colorful produce, and key vitamins provide the raw materials that keep the antioxidant cycle alive.
And where lifestyle alone may not be enough, we can support the system: with precursors like NAC and glycine — and, in modern settings, with clinical delivery methods that restore what diabetes so often drains.
Individually, these steps may seem modest. Taken together, they form a strategy — a way of shifting the body from vulnerability toward balance, and from progression toward protection.
The Takeaway
Type 2 diabetes is not just a disease of sugar, but of stress — oxidative stress.
Glutathione stands at the intersection of metabolism, insulin resistance, and long-term complications.
Strengthening this system through lifestyle, precursor supplementation, and, where appropriate, modern delivery methods may not cure diabetes, but it offers a way to slow its progression, protect vulnerable organs, and reshape metabolic health for the long run.
Summary
- Diabetes doesn’t only deplete GSH — it impairs enzymes in the glutathione system (like glutathione synthetase, γ-glutamylcysteine synthetase, glutathione peroxidase).
- This means the problem is not only “not enough fuel,” but also “broken machinery.”
- GSH (Glutathione) depletion links directly to vascular dysfunction, neuropathy, nephropathy, and retinopathy. It plays a role in chronic inflammation, a driver of long-term diabetic damage.
- Clinical pilot studies (e.g., Kumar et al.) showed improved mitochondrial function, lowered oxidative stress, and better insulin sensitivity in older adults with GlyNAC. The review stresses that while promising, large RCTs are missing.
- Besides exercise and nutrition, the paper also highlights weight loss, caloric restriction, and metabolic flexibility as key strategies to reduce oxidative load and improve glutathione recycling.
- Sleep and circadian rhythm were mentioned as underexplored but relevant areas for glutathione regulation.
- Low GSH is not just a “consequence” of insulin resistance — it may also feed the cycle, worsening mitochondrial dysfunction and impairing insulin signaling. This sets up a vicious loop: hyperglycemia → oxidative stress → low GSH → worse insulin resistance → more hyperglycemia.
Reference
Tuell JL, Bhattacharya D, Leeuwenburgh C, Chaudhuri A, Kumar V. The Role of Glutathione and Its Precursors in Type 2 Diabetes. Antioxidants (Basel). 2024 Feb;13(2):203. doi:10.3390/antiox13020203. PMID: 38398493; PMCID: PMC10885928.
Disclaimer: These statements are for informational purposes only and have not been evaluated by the Food and Drug Administration. This content is not intended to diagnose,treat, cure, or prevent any disease. Always consult a licensed healthcare provider before starting any supplement or therapy.

Written by Elena Brull, FNR, Functional Nutrition Researcher & Women’s Health Journalist
About the Author
Elena Brull, FNR, is a Functional Nutrition Researcher and Women’s Health Journalist specializing in integrative approaches to hormonal balance, nutrition, and longevity. Her work combines evidence-based insights with holistic health principles to help women understand their biology and live in rhythm with it. She writes from a non-clinical, educational perspective — with the intention to inform and empower, not to diagnose or prescribe.